Travelling This Road: What the 50% Travel Cap Means for Allied Health and Participants.
When travel cuts drive therapists away, who really pays the price?
If you’ve felt a disturbance in the force this month, in a rare and beautiful act of administrative punctuality, the NDIS actually released the new price guide more than 1 day before the financial year began. But double the lead time has translated into double the panic because it included some cost cutting measures that might just derail an entire sector.
From 1 July 2025, the NDIA introduced a significant change: allied health professionals can now only claim 50% of their hourly rate for travel time. That means for every minute spent getting to or from a participant, they’ll can only claim at half the hourly rate they usually charge for therapy.
For some, it’s a budget tweak. For others particularly mobile therapists, and regional practitioners — it’s a financial rug pull. Because unlike big providers who may have admin buffers and inner-city client clusters, a lot of allied health professionals drive… a lot. And they now have two weeks to figure out a new price model that won’t require a degree in creative accounting or subsidising their income with an OnlyFans account called ‘Feet, Forms & Functional Goals.
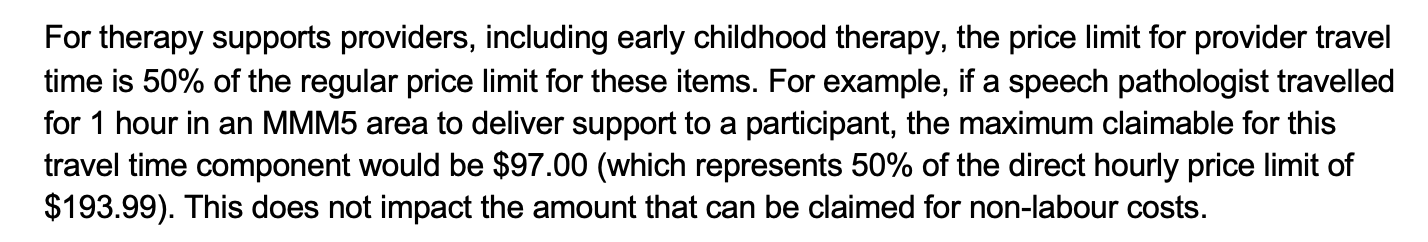
The way this is described in the latest NDIS Pricing Arrangements and Price Limits (previously the NDIS Price Guide) AKA the PAPL is as follows on Page 22;
This also applies for participants in Remote and Very Remote areas as follows (Page 26);
And while the description states this new rule applies for ‘Therapists’ which we generally equate to Capacity Building - Improved Daily Living, the PAPL also states that this includes support under Capacity Building – Improved Relationships (Page 84)
And for support under Capacity Building - Improved Health and Wellbeing (Page 87);
“If I Don’t Charge a Gap, I Can’t Afford to Work”
Allied health practitioners are increasingly facing a brutal choice:
Absorb the travel cut and risk running at a loss,
Stop offering mobile and outreach services altogether or
Start charging gap fees to some or all participants.
Some providers have already begun raising their standard hourly rate above the NDIS price limit or figuring out how to apply a ‘gap payment’. Others are grappling with the ethical dilemma of equity: is it fair that wealth determines access to best-practice therapy?
One therapist very understandably told me, “If I don’t increase my fees, I send the message that the current pricing is fine. It’s not. But if I do increase my rates, I price out the very people I want to support.”
Another clinician put it more bluntly: “I can’t afford to drive 45 minutes each way to see a client and walk away with less than minimum wage. That’s not sustainable. That’s charity.”
And it makes sense! How many years can pricing remain static while the cost of living feels like nightmare fuel for anyone who owns a calculator.
Regardless of our views on pricing - we have to get real about the outcomes of this new rule. Fewer providers offering mobile visits. More participants being told to travel — even when they can’t. And yet another quiet erosion of access for people with complex needs, low transport capacity, or limited support networks.
Because when the price guide pushes outreach out of reach, it’s not just the therapist who pays — it’s the families who can’t afford to fill the gap.
Are We Heading Towards a Two-Tier Allied Health System?
It’s starting to look that way.
On one side: providers who stick to the NDIS Price Arrangements and Price Limits (PAPL) — either because they’re registered or work exclusively with plan- and agency-managed participants.
On the other: clinicians who charge above the price limit and only work with self-managed clients — those who can afford to cover the difference out of pocket.
This creates a two-speed market:
A “public tier”, with capped rates and potentially reduced services,
And a “private tier”, with greater access — if you can pay for it.
That’s not what the NDIS was supposed to be.
To add to the confusion, Core providers are still able to charge their full hourly rate for Provider Travel, while therapists cannot. I’d love to understand the rationale behind this but I expect its related to SCHADS Award obligations which we definitely don’t have time to unpack today.
Hey Siri: Can Providers Charge Different Rates Based on Plan Type?
Don’t ask Siri cause she doesn’t know.
I don’t even know and I’ve scoured every policy, guideline and footnote I can find.
There’s plenty of guidance that clearly says you can’t charge NDIS participants more than non-NDIS clients - but when it comes to charging different rates within the Scheme? Like, say, charging a higher fee to self-managed participants compared to plan- or agency-managed ones? Crickets. I can’t find anything in writing that explicitly rules it out.
What we do know;
NDIS-registered providers: must stick to the PAPL. Full stop.
Plan managers: can only pay invoices up to the capped rate.
Self-managed participants: can agree to higher fees — but they must knowingly consent.
There are expectations about fairness, transparency, and not exploiting participants just because they’re on the NDIS. I can’t find any rule stopping a provider from charging a self-managed client more.
But that may change very soon!
Watch this space I guess…
Can I Pay a Gap Fee from Our Plan?
The answer? It depends — on what its for, how your plan is managed and who your provider is.
1. NDIS-Registered Providers
If a provider is registered with the NDIS, they must charge in alignment the PAPL price caps — no exceptions. That’s made clear on page 10 of the NDIS Pricing Arrangements and Price Limits 2025–26 (v1.0):
“Registered providers must comply with the NDIS Pricing Arrangements and Price Limits when making a payment request via the myplace provider portal.”
2. Plan-Managed Participants
Plan managers can only pay invoices that are within the PAPL price caps. So even if you give the green light to a higher fee, they legally can’t pay it from your plan.
(Page 11 of the Pricing Arrangements confirms this.)
3. Self-Managed Participants
This is where things get hectic. Self-managed participants can agree to pay above the price cap — but only if:
They give informed, voluntary consent
The fee is clearly communicated upfront
The provider isn’t exploiting their flexibility
They’re still spending in line with their NDIS plan and in line with the Can I Buy It checklist.
There’s no current written rule (that I’ve found) that explicitly bans a provider from charging self-managed clients more than plan- or agency-managed ones. But if you’re doing it? Document the conversation. Make sure consent is real, not implied. And maybe avoid calling it “admin fees” (because that’s not allowed — see below).
Real-World Scenarios Impacted by the New 50% Travel Rule
When provider travel is clinically required — like visiting home and school to assess function across environments. Should the clinician send a drone in to assess classroom accommodations remotely?
When a participant is learning to cook a meal — they need to practise in their own kitchen, using their own stove, fridge, and bench height. It can’t be done in the clinic.
When a participant is working on personal hygiene like showering independently — because the actual bathroom layout, equipment setup, and water temperature matter
When a child is building morning routine skills — and the OT needs to see the actual chaos of school-day mornings, not role play it in a pretend bedroom or a sensory gym
When the participant is trialling assistive tech or home modifications — because you can’t test equipment in a vacuum. It has to work in the participant’s real-world setup.
When the person is learning to safely navigate stairs, doorways, or flooring in their home — the clinic may have ramps and elevators, but the participant’s house has stairs and rugs.
When a participant uses a customised communication system (AAC, switches, or eye-gaze tech) — the setup at home is often unique and must be part of the therapy
When support needs to include the whole family — and sessions need to involve siblings, carers and shared spaces
When the participant doesn’t have a modified vehicle and literally can’t attend community clinics without three support workers and a teleportation device.
When the participant requires hoisting, positioning equipment, or other supports none of which fits neatly into the boot of your average Corolla.
When the child has sensory or behavioural needs that make community access overwhelming or unsafe for both child and carer
When multiple services are delivered in-home as part of an integrated, collaborative therapy model (e.g. co-visits, joint team care meetings and goal planning)
When the participant lives in a rural, regional or outer-suburban area where local providers don’t exist or are fully booked until the next federal election.
When a family has multiple children with disability and the logistics of therapy appointments would make your Google Calendar cry.
When a participant is in crisis, traumatised or disengaging and won’t reliably access centre-based supports - this creates a huge risk of complete disengagement.
Here is where the logic breaks down entirely: It might cost the NDIS more, not less
When provider travel is underpaid — or scrapped altogether — families are left scrambling to figure out plan B. And here’s where the maths gets messy.
If a therapist can’t offer sessions in the participants community settings, participants may have to rely on support workers to get to and from the clinic. That means:
More hours of Core funding used (usually around $70/hr)
Less clinical time in the home — where many goals actually happen
More emotional and logistical pressure on families just trying to make it work
Let’s break it down.
Scenario 1: Using Support Workers for Transport
For a 1-hour therapy session, with 30 minutes of travel:
1 hr therapy @ $193.99
2 hrs of support worker transport @ $70/hr = $140
Total = $333.99
And we haven’t included the kms (Activity Based Transport) that will also be charged to the participants plan here.
Scenario 2: Old Model with Full Travel Rate
1 hr therapy @ $193.99
30 mins travel @ $193.99/hr = $96.99 (Plus kms if the provider charges these)
Total = around $290.98
That’s a $43 increase per session — just to shift the costs from one funding category to another. Same outcome (a participant accessing therapy), just with more logistical chaos and higher costs to the Scheme.
Systemic Inefficiencies Galore
Support workers are not taxi drivers — it’s a poor use of qualified staff
Families are left to coordinate transport, often at the cost of their own employment
Clinical outcomes may be reduced when therapy is removed from the participant’s natural environment
And… the age old question - will the NDIS increase Core funding to account for the higher need to attend the clinical setting?
Just don’t hold your breath my friend.
Finally, parents will have to take time away from work and their other responsibilities to drive their child to and from therapy appointments - impacting financial and employment stability and further disadvantaging families who already face increased costs and reduced earning capacity due to their child’s disability.
Those same parents will have no choice but to drag younger siblings along to the clinical setting — and it’s hard for a parent and child to focus on a therapy session when their 18 month old is chewing the door handle or losing their shiz because its their nap time. For some kids this will absolutely result in a loss of meaningful clinical engagement and skill building that occurs in the participant’s own environment
This is a textbook case of a policy that looks cheaper on paper but costs more in practice — not just financially, but in accessibility, equity, and real-world outcomes.
So What Happens Next?
If this change leads to widespread gap payments, here’s what we’re really looking at:
Participants in regional and outer-metro areas may lose access to mobile supports entirely. No travel funding = no outreach. Simple as that.
More services will be centralised, and support workers will end up as glorified taxi drivers — instead of providing meaningful, goal-focused support.
More participants will be nudged toward self-management — not because it suits them, but because it’s the only way to pay gap fees. Meanwhile, those who don’t have the capacity self-manage (because of age, disability, or circumstance) will be left with fewer choices for support.
Families will be forced to pay more, or settle for less — while therapists juggle the ethics of charging gap fees against the reality of running a viable business.
wWe reinforce a quiet but insidious idea: that only the wealthy should get the best care in the places that are most effective and beneficial for them.
And in a final twist: the NDIA may decide to publish or clarify policy stating that providers cannot charge self-managed participants more than others.
💡 What Can Be Done?
Therapists: Be upfront and give plenty of notice.
If you're introducing a gap fee, explain why — and explain what it covers. Participants need that clarity to determine whether they can claim it from their plan (and yes, that often depends on how it’s worded on the invoice).
Publishing a clear, accessible statement outlining your pricing policy and values could be a great start.
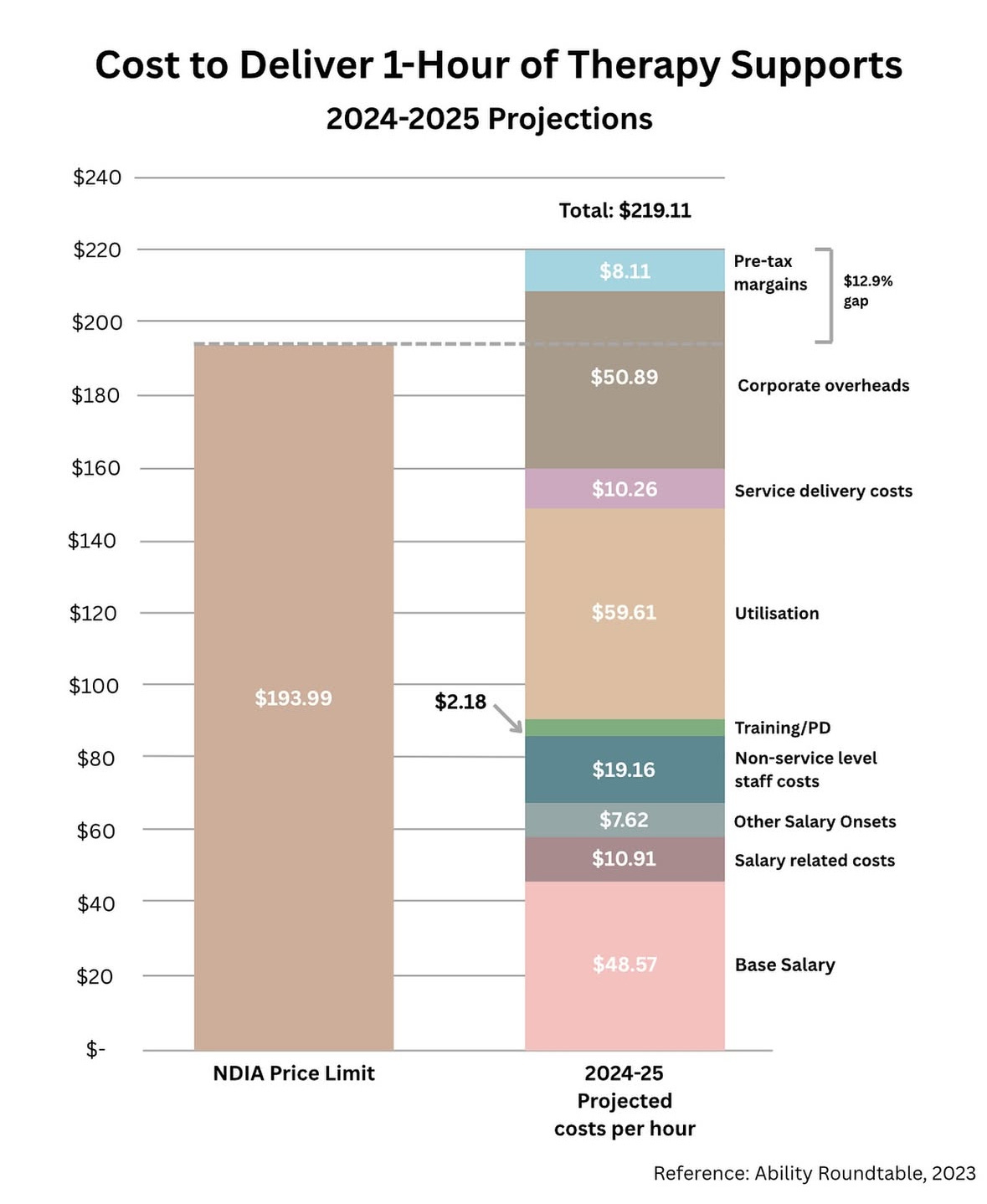
There is a great visual circulating with a breakdown of what one hour of therapy costs;
So where does that money actually go? Here’s the breakdown:
$48.57 – Average therapist’s base wage
$10.91 – Superannuation, leave, payroll tax etc
$7.62 – Other wage-related costs
$19.16 – Non-client-facing staff (admin, management)
$59.61 – Utilisation costs:
Supervision, governance, non-billable admin, prep time, compliance and safeguarding requirements, and the joy of school holiday schedule gaps$10.26 – Therapy materials and equipment
$50.89 – Corporate overheads: rent, insurance, registration, workers comp
$8.11 – Pre-tax margin (aka “profit,” assuming nothing unexpected eats it first 🙃)
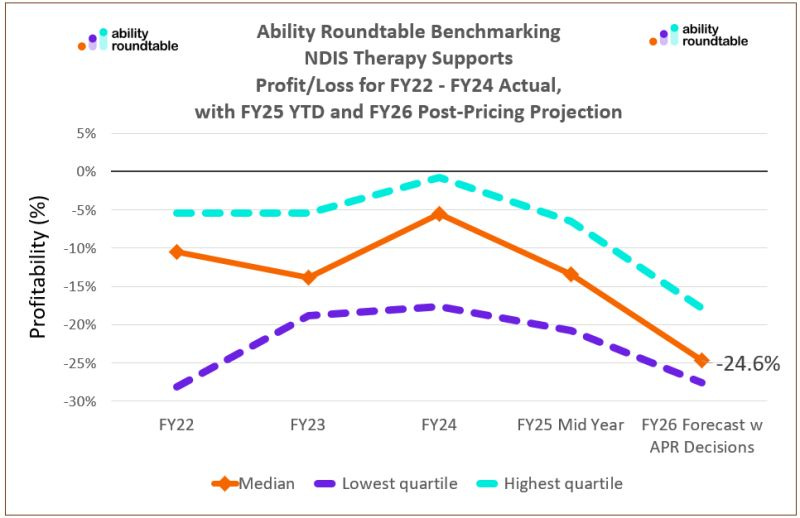
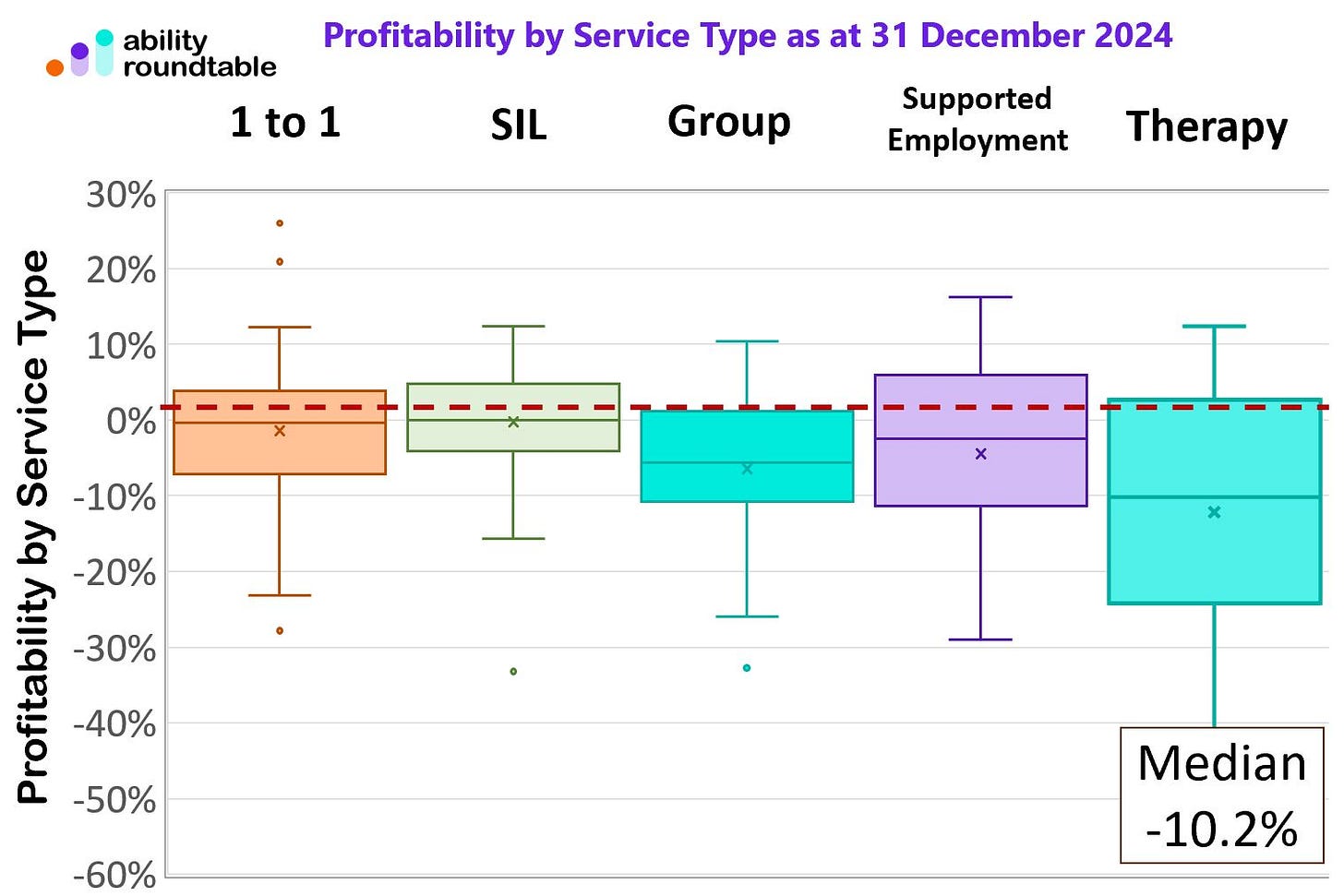
Ability Roundtable also showed us how dire profit margins are in the sector right now, and it wasn’t pretty for anyone who likes to be able to pay their bills and keep food on the table;
Also consider:
Being super transparent about how you structure your sessions and what’s included in all fees
Clarifying how much of your time goes toward planning, documentation, and communication — not just face-to-face therapy
If you’re absorbing travel costs, let clients know that too. They deserve to understand the real cost of best-practice support — and the gap between that and what the NDIS is willing to fund.
Ensure you have a really strong understanding of what can be charged under Non Face to Face Support. Admin costs and the costs of being business can not be charged to an NDIS plan. The PAPL states on page 32:
Participants and Carers: Ask questions. What do these travel changes mean for your access to therapy? Is the provider introducing gap fees? Can you negotiate an hourly rate to help you avoid out-of-pocket costs — while still staying compliant with the PAPL?
If you're self-managed, check whether your plan is flexible enough to absorb small increases. If you're plan-managed, your plan manager can help you understand what's claimable — and what’s not.
And if your access is being impacted by these changes? Say something. Raise it with your LAC, your support coordinator, or your MP. Gap fees might be framed as a provider issue but their root cause and the issues they create is structural. And structural issues need systemic fixes.
And yes — there’s still hope. Peak bodies, professional associations, and advocacy organisations are pushing back loudly. They’re meeting with Members of Parliament and helping to share real stories of how detrimental this changes are. Conversations are happening with the NDIA and DSS. Whether it’s a policy walk-back or a travel loading rethink, this isn’t over yet.
Resources for Providers and Therapists;
This is a time of unprecedented advocacy. Every Peak Body in Australia, Speechies,
Dieticians, Osteopaths, Physiotherapists, Occupational Therapists, Psychologists, Podiatrists, Exercise Physiologists and Behaviour Practitioners are speaking up loudly about how harmful these cost cuts are. The sector has power in unity and while the Government might be emboldened right now by their recent election win, advocates are highlighting this move is a huge mistake based on flawed data.
🔹 Change.org Petition + Survey
39K signatures and counting! Add your name and share your experience of how the 50% travel cap is affecting your clients and your practice.
👉 Sign and share the petition here
🔹 Allied Health Professions Australia (AHPA)
Peak national organisation representing allied health — they’re coordinating formal responses and policy engagement.
Visit AHPA
🔹 Occupational Therapy Australia
OTA is actively advocating for fair and sustainable pricing through DSS and the NDIA. Add your voice or stay updated.
Visit OTA
🔹 Speech Pathology Australia
SPA is collecting member feedback and engaging directly with NDIS policymakers.
Visit SPA
🔹 Australian Psychological Society (APS)
For psychologists affected by the changes — check their NDIS advocacy updates and contact channels.
Visit APS
🗂️ Bonus Tip: Document any client cancellations, reduced service access, or increased out-of-pocket costs resulting from the travel cap. Real-world examples strengthen the case for policy change.
Resources for Participants & Carers: Speak Up (If you have the capacity).
If these travel changes are affecting your access to therapy or increasing your out-of-pocket costs, you’re not alone — and you don’t have to stay quiet about it.
🔹 Change.org Petition + Survey
39K signatures and counting. Share how these changes are impacting you or your child. Your lived experience helps show the real-world consequences of policy decisions.
👉 Add your voice here
🔹 Advocating for Children with Disability Family Impact Survey (Therapy Travel Cap)
Designed for parents and carers to describe how the changes are affecting family routines, access to therapy, and plan budgets.
👉 Complete the parent survey here
🔹 Every Australian Counts
A grassroots movement fighting for a fair and accessible NDIS. Follow their updates or share your story.
Visit Every Australian Counts
🔹 Your Local MP
Not sure what to say? Just tell them how this change affects your family’s access to therapy. It doesn’t have to be fancy — it just has to be honest.
Find your federal MP
🔹 NDIS Quality and Safeguards Commission (if needed)
If you're concerned a provider is charging unfairly or without your informed consent, you can raise it here.
Visit the NDIS Commission
Tip: Keep a quick log of cancelled sessions, cost increases, or changes in therapy access. These notes can help if you need to request a plan reassessment — or explain why your Core budget just isn’t stretching like it used to.
📣 Final Thoughts
The NDIA might think it’s trimming travel fat — but it’s really cutting muscle. Allied health professionals are the engine room of functional improvement. And every minute not adequately compensated is another reason for great therapists to walk away from the sector altogether.
Some people argue providers already get paid enough. But where outreach is genuinely needed, it isn’t a luxury — it’s a lifeline.
And it’s especially vital for people living in more rural or remote areas where outreach may be the only option. These communities already face waitlists, workforce shortages, and geographic isolation. Now they’re also being disproportionally disadvantaged, absorbing the fallout from policy decisions made in rooms far removed from lived experience
Our decision makers need to recognise that we can’t save cents on travel, and lose entire therapy teams in the process.
Let’s not pretend we can drive quality outcomes at half-price fuel.
The Scheme was never meant to be a race to the bottom. It should be bold, accessible, drive innovation and meet on real-world need. So if we want to keep the best practitioners in the field, the funding needs to follow the function. Literally.
Till next time
x Anna